Cardiac Conduction System⁚ An Overview
The cardiac conduction system is a network of specialized cardiac muscle cells that initiate and transmit the electrical impulses responsible for the coordinated contractions of each cardiac cycle. The electrical conduction system of the heart includes the sinoatrial node, internodal pathways, atrioventricular node, bundle of His, bundle branches, and Purkinje fibers.
Introduction⁚ The Importance of Cardiac Conduction
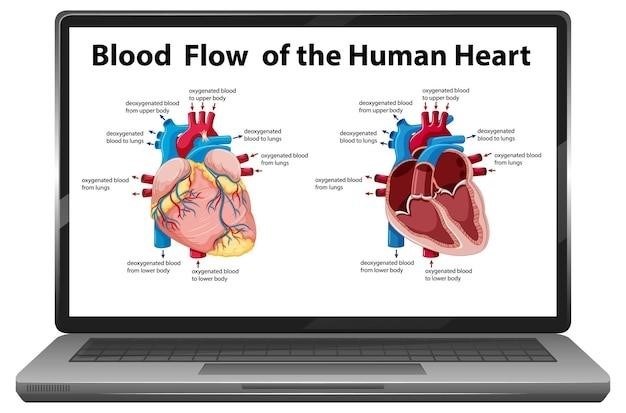
The human heart beats an astounding 2.5 billion times during a normal lifespan, a feat made possible by the intricate and vital system of cells known as the cardiac conduction system (CCS). This system is responsible for the generation and propagation of electrical impulses that orchestrate the rhythmic and synchronized contractions of the heart’s four chambers, ensuring the efficient pumping of blood throughout the body. The CCS is crucial for maintaining a steady heartbeat, regulating blood pressure, and supporting the vital functions of all organs;
Disruptions to the normal functioning of the CCS can lead to a wide range of cardiovascular problems, including arrhythmias, heart blocks, and other conduction disorders. These conditions can severely impact the heart’s ability to effectively pump blood, potentially leading to life-threatening complications. Understanding the intricate workings of the CCS is essential for diagnosing and treating these disorders.
This comprehensive guide delves into the anatomy, physiology, and clinical implications of the cardiac conduction system, providing a detailed overview of the key components, their roles in electrical impulse generation and propagation, and the impact of conduction system disorders on heart health. By gaining a deeper understanding of this vital system, we can better appreciate its significance in maintaining cardiovascular health and the potential consequences of its dysfunction.
Components of the Cardiac Conduction System
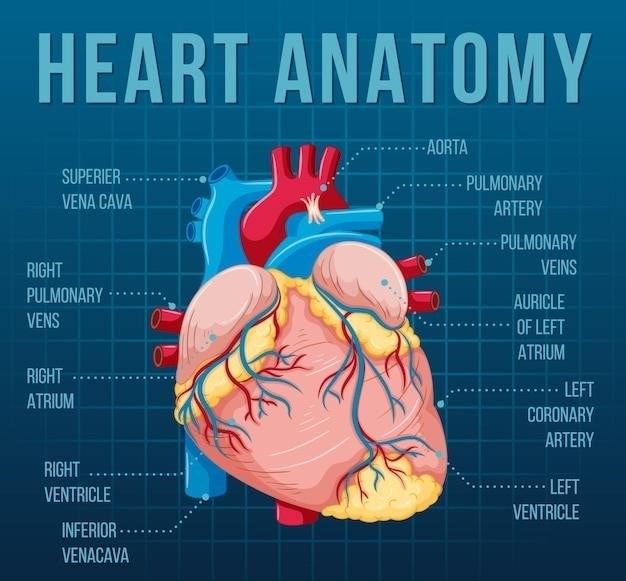
The cardiac conduction system is comprised of specialized cells that act as the heart’s internal electrical wiring, ensuring coordinated contraction of the atria and ventricles. This intricate network is made up of four primary components, each playing a critical role in initiating and transmitting electrical impulses throughout the heart⁚
2.1. Sinoatrial Node (SAN)
The sinoatrial node, located in the right atrium, acts as the heart’s natural pacemaker. Its cells possess the unique ability to spontaneously generate electrical impulses, setting the rhythm for the entire heart. These impulses, known as action potentials, spread through the atrial muscle, causing the atria to contract and pump blood into the ventricles.
2.Atrioventricular Node (AVN)
Situated at the junction of the atria and ventricles, the atrioventricular node acts as a gatekeeper, delaying the electrical impulse briefly before allowing it to proceed to the ventricles. This delay ensures that the atria have enough time to fully contract and empty their blood into the ventricles before the ventricles begin to contract.
2.3. Atrioventricular Bundle (Bundle of His)
The atrioventricular bundle, also known as the bundle of His, is a pathway that extends from the AV node into the interventricular septum, the wall separating the ventricles. This bundle divides into two branches, one for each ventricle, allowing the impulse to travel to both sides of the heart simultaneously.
2.4. Purkinje Fibers
The Purkinje fibers are a network of specialized conducting cells that branch extensively throughout the ventricular walls. These fibers rapidly transmit the electrical impulse to the ventricular muscle, triggering coordinated contraction of the ventricles and propelling blood to the lungs and the rest of the body.
2.1. Sinoatrial Node (SAN)
The sinoatrial node (SAN), often referred to as the heart’s natural pacemaker, is a small, specialized cluster of cells located in the right atrium, near the entrance of the superior vena cava. It plays a pivotal role in initiating and regulating the heart’s rhythmic beating. The SAN cells possess a unique property known as automaticity, meaning they can generate electrical impulses spontaneously without external stimulation. This intrinsic ability allows the SAN to set the pace for the entire heart.
The process begins with the spontaneous depolarization of SAN cells, which triggers an action potential, a brief electrical signal that travels through the heart. This action potential spreads through the atrial muscle, causing the atria to contract and pump blood into the ventricles. The rate at which the SAN generates these impulses determines the heart rate, which can be influenced by various factors such as the autonomic nervous system, hormones, and physical activity.
The SAN’s role in the heart’s rhythm is crucial. If the SAN malfunctions, the heart’s rhythm can become irregular or slow, potentially leading to various cardiac problems. Understanding the anatomy and function of the SAN is essential for diagnosing and treating a wide range of heart conditions.
2.2. Atrioventricular Node (AVN)
The atrioventricular node (AVN) is another crucial component of the cardiac conduction system, situated in the right atrium, near the junction of the atria and ventricles. Unlike the SAN, which spontaneously generates electrical impulses, the AVN acts as a gatekeeper, delaying the transmission of electrical signals from the atria to the ventricles. This delay is essential for proper heart function, ensuring that the atria have finished contracting and filling the ventricles with blood before the ventricles begin their own contraction.
The AVN’s role in coordinating the heart’s pumping action is critical. It acts as a buffer, preventing the rapid transmission of electrical impulses from the atria to the ventricles, which would disrupt the synchronized contraction of the heart. The AVN’s delay allows for a controlled and efficient filling of the ventricles, ensuring that the heart pumps blood effectively throughout the body.
The AVN’s function can be affected by various factors, including age, disease, and medications. When the AVN malfunctions, it can lead to heart block, a condition where the electrical impulses are delayed or blocked altogether, resulting in a slower heart rate or irregular heartbeat. Understanding the AVN’s structure and function is vital for diagnosing and treating heart rhythm disorders.
2.3. Atrioventricular Bundle (Bundle of His)
The atrioventricular bundle, commonly known as the Bundle of His, serves as the sole pathway for electrical impulses to travel from the atria to the ventricles. This specialized bundle of fibers originates from the AVN and descends into the interventricular septum, the wall that separates the left and right ventricles. The Bundle of His is essential for coordinating the contraction of the ventricles, ensuring that both chambers contract simultaneously and effectively pump blood out of the heart.
The Bundle of His is a critical component of the cardiac conduction system, responsible for transmitting electrical signals at a faster rate than the AVN. This rapid conduction is necessary for the synchronized contraction of the ventricles, which is essential for efficient blood circulation throughout the body. The Bundle of His also plays a crucial role in maintaining a consistent heart rhythm, ensuring that the ventricles contract in a regular and coordinated manner.
Disruptions to the Bundle of His can lead to various heart rhythm problems, including heart block, where the electrical signal is delayed or blocked, leading to a slower heart rate. Damage to the Bundle of His can occur due to various factors, including heart disease, surgery, or certain medications. Understanding the structure and function of the Bundle of His is essential for diagnosing and treating heart rhythm disorders.
2.4. Purkinje Fibers
Purkinje fibers, a specialized network of conductive cells, form the final stage of the cardiac conduction system, extending from the Bundle of His throughout the ventricular walls. These fibers, named after the Czech anatomist Jan Evangelista Purkinje who discovered them in 1839, are responsible for rapidly transmitting electrical impulses to the ventricular muscle cells, triggering their coordinated contraction. The Purkinje fibers are characterized by their large diameter and low resistance to electrical flow, enabling them to conduct impulses at remarkably high speeds, ensuring a rapid and synchronized contraction of the ventricles.
The Purkinje fibers are strategically located within the ventricular walls, branching extensively to reach every part of the ventricular muscle. This extensive distribution ensures that the electrical signal reaches all muscle cells simultaneously, leading to a coordinated contraction of the ventricles. The efficient and rapid conduction provided by the Purkinje fibers is essential for the forceful ejection of blood from the heart, propelling it throughout the body.
Damage to the Purkinje fibers, often due to heart disease or certain medications, can disrupt the efficient conduction of electrical impulses, leading to irregular heart rhythms. This can result in heart block, where the electrical signal is delayed or blocked, causing a slower heart rate, or ventricular fibrillation, a life-threatening condition where the ventricles contract chaotically. Understanding the structure and function of the Purkinje fibers is crucial for diagnosing and treating heart rhythm disorders.
Electrical Impulse Generation and Propagation
The rhythmic beating of the heart is a complex process orchestrated by the intricate interplay of electrical impulses generated and propagated through the cardiac conduction system. This system acts as the heart’s electrical wiring, ensuring a coordinated contraction of the atria and ventricles, enabling efficient blood circulation. The process begins with the spontaneous generation of electrical impulses in the sinoatrial node (SAN), the heart’s natural pacemaker, located in the right atrium. This electrical signal, initiated by specialized pacemaker cells, triggers a wave of depolarization that spreads across the atrial muscle, causing it to contract.
The electrical impulse then travels to the atrioventricular node (AVN), situated at the junction between the atria and ventricles. Here, the signal is briefly delayed, allowing the atria to complete their contraction before the ventricles are stimulated. This delay is essential for ensuring efficient blood flow from the atria to the ventricles. From the AVN, the electrical impulse travels down the atrioventricular bundle (Bundle of His), a specialized pathway that connects the atria and ventricles. The bundle then branches into two bundle branches, which carry the signal to the left and right ventricles respectively.
Finally, the electrical impulse reaches the Purkinje fibers, a network of conductive cells that distribute the signal throughout the ventricular muscle. The rapid conduction of the electrical impulse through the Purkinje fibers ensures a synchronized contraction of the ventricles, propelling blood into the aorta and pulmonary arteries. This intricate process of impulse generation and propagation is essential for the efficient and rhythmic pumping action of the heart, sustaining life by circulating blood throughout the body.
Clinical Implications of Conduction System Disorders
Disruptions in the normal function of the cardiac conduction system can lead to a range of cardiovascular disorders, impacting the heart’s ability to pump blood effectively. These conduction system disorders can manifest as arrhythmias, characterized by irregular heartbeats, or heart blocks, where the electrical signal is delayed or blocked entirely. Arrhythmias can range from benign to life-threatening, and may cause symptoms like palpitations, dizziness, or shortness of breath. In severe cases, they can lead to heart failure or stroke.
Heart blocks, on the other hand, can cause the heart to beat slowly, leading to fatigue, lightheadedness, and even fainting. The severity of heart block varies, with some individuals experiencing mild symptoms while others require a pacemaker to maintain a regular heart rhythm. The diagnosis of conduction system disorders relies on a combination of physical examination, electrocardiogram (ECG), and other specialized tests. Treatment options may include lifestyle modifications, medications, or in some cases, surgical procedures like pacemaker implantation or ablation therapy.
Understanding the clinical implications of conduction system disorders is crucial for early diagnosis and effective management. Regular check-ups, particularly for individuals with known risk factors such as family history of heart disease or certain medical conditions, are essential for detecting early signs of conduction system problems. Timely intervention can significantly improve the prognosis and quality of life for patients with these disorders.
Research and Future Directions
Despite significant advances in understanding the cardiac conduction system, ongoing research continues to explore its intricacies and seek innovative solutions for related disorders. One key area of focus is the development of novel therapeutic approaches for arrhythmias and heart blocks. This includes exploring new drug therapies, biocompatible materials for pacemakers and implantable devices, and personalized treatment strategies based on genetic and electrophysiological profiles.
Another promising research avenue involves the use of stem cell therapy to regenerate damaged conduction system cells. Researchers are investigating the potential of stem cells to differentiate into specialized cardiac cells, potentially restoring normal electrical function in individuals with conduction system disorders. Additionally, ongoing research is investigating the role of gene therapy in modifying the electrical properties of heart cells, aiming to prevent or correct conduction system abnormalities.
Furthermore, the development of advanced imaging techniques and computational modeling tools is enhancing our understanding of the complex electrical activity within the heart. These advancements are enabling researchers to better visualize the intricate network of conduction pathways, analyze the propagation of electrical impulses, and identify potential targets for therapeutic interventions. As research progresses, we can expect to see even more innovative treatments and personalized approaches to manage conduction system disorders, ultimately improving the lives of patients worldwide.